Our health ministry appears to hide from declaring sporadic infection despite all the obvious evidences. It still continue responding the usual way that had proven to be absolutely ineffective. If effective, then the infections should reduce, not increase, so the only sane conclusion is that it is not effective. If we continue with this ineffective methods, it is not just stupid but reckless and dangerous.
What is sporadic infection? It is just an infection that cannot be traced where it comes from. That is why the Ministry reclassify the previously unknown case as non-sporadic because it was traced to the Tabligh gathering. Is it correct?
Just because you can trace to a broad location, does not mean that it is already traced. For example, someone in Brunei contracts an infection while in Malaysia. Brunei is still considered as traceable but not Malaysia, as far as Brunei is concerned.
For Malaysia to consider the infection traceable, it has to track where the Brunei person got the infection and who? 16 people in Brunei contracted the Covid19, and each one must be traceable in Malaysia in order for the case to be a non-sporadic infection.
Our Ministry can claim that it had managed to trace it to the Tabligh gathering of 12,500 Malaysians ( or 5,000). Provided these people remain static and remains in that mosque, then we can call it traced infection, but unfortunately, all had gone away. So for all the 16 infections in Brunei traced to the Tabligh gathering, there are already 16 untraceable or sporadic infections occurring at the mosque.
350 of them had gone back to Sabah, and 3 were already traced back to the tabligh. Provided all 350 had been tested by now and most are negative, Sabah can still claim to have no sporadic infection. I doubt it. With insufficient test kits and difficulty in contacting these attendants and their families, it will led to sporadic infections sooner or later.
For West Malaysia, it is too late already. But Sabah is still safe so the trick is to isolate all the infections regionally, or state by state, so that it can be tackled with more stringent measures, that needs to be applied to all of Malaysia.
Why sporadic infection is dangerous? Since we do not know where the infection starts, it means that anyone can be the spreader or pre-spreaders and so on. In the US, it is called silently spreading in the community for weeks. With a mean incubation period of just less than 4 days, and 80% are mild, this is where the danger lies.
These 80% mild cases are the spreaders without even knowing about it. They will lead to the death of the 20% because no more hospital facilities, and later the deaths of the 80% also when there is no more food and transportation.
Can hospitals be overwhelmed? Already happened in Wuhan and Lombardy. But the maths is very clear. Malaysia has a population of 30 million. 20% of 30 million is 6 million. How many ventilators and beds do we have to let these 6 million live? At most we have 6,000 machines and beds all over Malaysia. 6,000 divided by 6 million is 0.1%, so only 0.1% will survive.
Oh, not all 6 million will be infected in 2 weeks, the duration of the use of the machines. Or we can extend to ten times, i.e. 20 weeks, which is 5 months. Just look at the rate of growth in Lombardy and Wuhan. They were using quarantines and tracing also, just like Malaysia now, but it was too late for them.
Still, it is only 1% that will survive, 99% of 6 million will die.
This is assuming there are still doctors who can man these 6,000 machines throughout the 20 weeks.
Malaysia, trying to use the same methods, will meet exactly the same fate. Thinking that Malaysia is different, despite using the same methods, is just folly and not proven by facts on the ground.
The only proven method is complete lockdown like in Hubei province. But we can prevent this if we can act quickly and intelligently by admitting to the facts that Covid19 can spread without any symptoms which also means that it is aerobic.
Covid-19: Experts call for speedier, urgent response
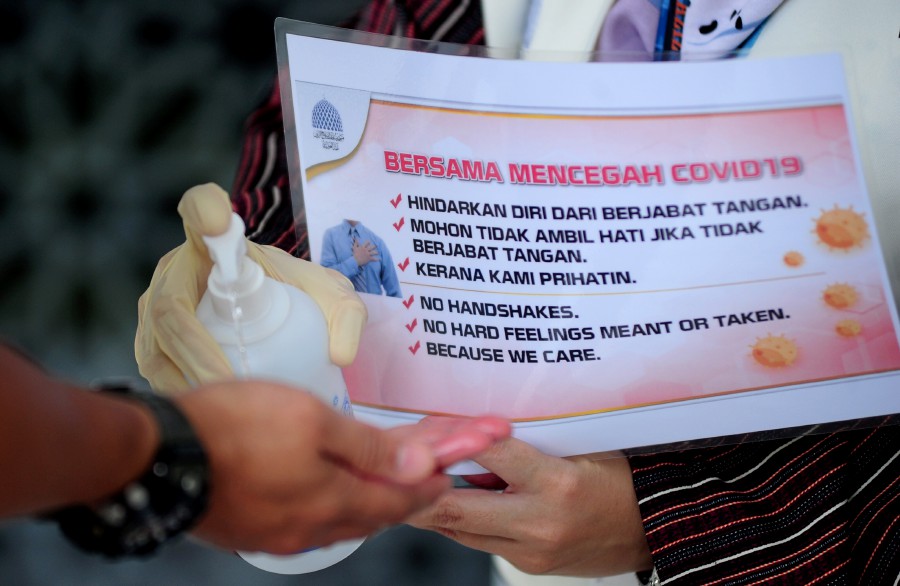
A staff at Sultan Salahuddin Abdul Aziz Shah mosque in Shah Alam, squeezes out hand sanitiser on to a palm of a person, amid the Covid-19 coronavirus outbreak. - BERNAMA pic
KUALA LUMPUR: Medical experts are urging for faster and urgent action in handling the Covid-19 outbreak in the country.
This follows the World Health Organisation’s declaration of the disease as a pandemic on Wednesday, and the tabligh gathering at the Seri Petaling Mosque here recently, which sparked a new cluster transmission of Covid-19 in the country.
Dr Ong Hean Teik, past chairman of the Penang branch of the Malaysian Medical Association, said the situation in Malaysia was severe and this warranted stricter measures.
This, he said, included banning mass gatherings, postponing weddings and events, as well as closing down schools temporarily in high-risk areas.
“The virus is present in the community. We not only have cluster cases (sparked by Cases 26 and 131), but we have also entered the community transmission stage, which calls for the authorities to boost its emergency response mechanism.
“Issuing an advisory is not enough. The Health Ministry should be clear in conveying the seriousness of the outbreak.
“Malaysia was successful in containing the spread during the first wave. Case 26 changed this. Since Cases 26 and 131 contracted the virus in Malaysia, isn’t it enough to indicate community spread?
“People need to be informed to contain the virus.”
Dr Ong, a consultant cardiologist and past president of Penang Medical Practitioners’ Society, said medical practitioners, including head of departments at public hospitals, had raised concern about the shortage of Covid-19 test kits.
This, he said, was causing a backlog in case detection, especially following the tabligh gathering where thousands of people were scrambling to get tested.
He questioned if the ministry had adequate resources in place if the outbreak worsened.

“WHO’s data suggests that 80 per cent of Covid-19 infections are mild or asymptomatic, 15 per cent are severe infections requiring oxygen and five per cent are critical infections requiring ventilation.
“How many ventilators and extracorporeal membrane oxygenation machines do we have for those with respiratory failures? Do we have sufficient protective gear for medical personnel?”
Former Malaysian Medical Association president Datuk Dr N.K.S. Tharmaseelan agreed that Malaysia had entered the community transmission stage. He advised the public to take extra precautions.
Malaysian Public Health Medicine Specialist Association president Datuk Dr Zainal Ariffin Omar said the Health Ministry should make public the list of places that Covid-19 patients had visited, worked at or areas they lived in.
This, he said, was so that the public could practise social distancing.
Paediatrician Datuk Dr Musa Mohd Nordin said the asymptomatic transmission of Covid-19 made total containment difficult and problematic.
He said there might be a need to realign and reconsider some of the Health Ministry’s strategies of containment and mitigation.
“I do not think we need to follow the lockdown methodology of China and Italy. South Korea has been successful in reducing the number of confirmed cases of Covid-19 from 900 per day to fewer than 100 per day.
“We can learn from South Korea’s strategy. We must ensure that there are sufficient diagnostic test kits.
“South Korea undertakes 12,000 to 20,000 tests per day.
“To facilitate testing, South Korea has set up drive-through Covid-19 test centres. This drive-through model has been replicated by KPJ Damansara Specialist Hospital (KPJ-DSH) and Sungai Buloh Hospital.
“KPJ-DSH has operated drive-through test centres at the premises of government-linked companies to test those who had close contact with Case 26.”
Dr Musa said it was crucial to be transparent in information sharing because access to accurate information could debunk fake news and fearmongering.
“It empowers the people to be active partners of the Health Ministry and the government in the fight against the outbreak.”
No comments:
Post a Comment